Hemorrhoids are the blood vessels located in the last part of the rectum and the anus. They are made of "bearings" and placed on the anus in an external area (external hemorrhoids) and in an inner area (internal hemorrhoids).
The mucous prolapse of the rectum is predominantly the outflow from the anus of the rectal mucosa, that is, the inner lining of the rectum comprehensive of internal hemorroids, during defecation.
INDEX:
1. WHAT THE HEMORROIDS ARE
2. THE CAUSES OF HEMORROIDS
3. PROCEDURE FOR DIAGNOSIS
4. SURGICAL TECHNIQUES FOR HEMORROID TREATMENT
5. POST-OPERATIVE INSTRUCTION AFTER HEMORROIDS AND PROLAPSE TREATMENT
1. WHAT THE HEMORROIDS ARE
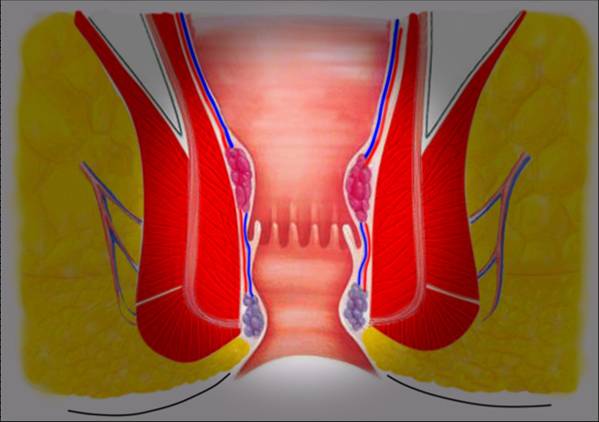
Hemorrhoids are the blood vessels located in the last part of the rectum and anus. They are made of "bearings" and placed on the anus in an external area (external hemorrhoids) and in an inner area (internal hemorrhoids).
2. THE CAUSES OF HEMORROIDS
Various are the causes for which hemorrhoids can inflate, swell and even escape from the anus (the so-called hemorrhoid and rectal prolapse). Excessive and repeated efforts to evacuate, chronic colitis, the habit of staying too long on the water, excessive hygiene, some liver or infectious diseases can cause all of the symptoms related to hemorrhoids such as anal pain, Bleeding, itching, swelling or loss. For the fear of being operated or simply modest (many people are ashamed of the visit) they often try to treat this pathology by one of the many methods popularized by us: The ointments, ice cold ice cubes etc that are mostly ineffective and even damaging. However, I would like to warn people who are affected, overlooked! Anal bleeding, mucus or pain can mask the symptoms of much more severe pathologies, such as rectal prolapse, polyps or rectum and colon cancers.
3. PROCEDURE FOR DIAGNOSIS
A simple specialist visit completed by anoscopy, in a few minutes, can exclude most other pathologies. However, a diagnosis of hemorrhoids does not mean intervention: 90% of people, men and women who are studying for hemorrhoids are NOT working and are treated only with health, nutrition and medicine advice. For those who have been overlooked for too long and do not respond to medical treatment, surgery is proposed.
4. SURGICAL TECHNIQUES FOR HEMORROID TREATMENT
The type of surgical treatment depends largely on the type and degree of hemorrhoids. It goes from the simple elastic binding of a single haemorrhagic cheetah that is performed ambulantly to more complex interventions. At present, the aim is to respect as much as possible the integrity of the anus and to improve the post-operative course by reducing the pain. Fear of pain is the one that terrorizes most people who are in charge of any intervention but for hemorrhoids this fear is amplified by the cultural legacy that has been handed down to us by generations of people who have undergone hemorrhoids and have disastrous experience . It's no longer so! For many years, the greatest attention of surgeons has been to carry out the least invasive surgery, which reduces post-operative pain and returns the patient to a normal life as fast as possible. It was an Italian, Prof. Antonio Longo, who about 15 years ago offered an intervention as an alternative to classical surgery with cuts on the anus for the removal of hemorrhoids. The intervention of Longo, on the other hand, respects the integrity of the anus and with a special apparatus cuts and stings a mucous tract inside where the hemorrhoidal veins pass. This section falls into an area that is not innervated by painful fibers. The result is exceptional: the inner seam pulls up the hemorrhoids, which no longer get blood from the broken veins, they leak. All without the classic pain of anal wounds, with only one night of hospitalization and a quick return to their activities. Seaming is performed with titanium microscopic clips that are partially integrated and partly exploded in the months following the intervention. For about 10 years, when conditions permit, Longo also called Hemorrhoids and I had the privilege of developing the technique in Hamburg and Vienna directly in the research and work places of Prof. Longo.
In recent years there have been many scientific studies on the subject. It has been shown that most of the hemorrhoidal diseases depend on prolapse. Internal hemorrhoids are located beneath the rectum mucosa. In the presence of a prolapse and during defecation are pushed out. There may be a single puddle, but in most cases it is more jerky to escape from the anus to simulate a kind of small cauliflower. As is the case: Imagine putting the sleeve of a jacket in which the inner lining is very abundant. This will leak out of the sleeve. The lining is the rectum mucosa, the sleeve is the rectum musculature. When lacerating and missing the fissure means, the fibrous ties between the mucous membrane and the musculature, the mucous membrane is dragged out of the anus by carrying the hemorrhoids and causing the so-called mucosal prolapse. At first, prolapse and hemorrhoids spontaneously fall within after defecation. Then the patient will have to reintroduce them manually during the wash. Afterwards, the sagged part is so inflamed that it can remain fixed outward with all the inconvenience of the case.
- Pain, anal and rectal burning, especially if you do not follow the analgesic schedule.
- Sense of weight and incomplete evacuation with frequent stimuli (called defecatory urgency). They are annoying sensations caused by internal swelling and irritation inside the anus. It only deals with pain relieve drugs and anti-inflammatory suppositories and decreases in about 15 days and disappears in about 30-60 days.
- Ecchymosis (blackish color of the perianal area) which disappears in about two weeks.
- Anal swelling at the hemorrhoids site. In his case the prolapse was predominantly treated. Any Skin tags and external hemorrhoidseventually present will undergo a physiological edema and congestion that regresses in a few days and disappears in about 6 months. During this period, episodes of thrombosis of the hemorrhoidal (swelling of a hemorrhoid that occurs as a hard ball for about 15 days are possible, and then regressed). Only after this period can any residues be removed by local anesthesia.
- Loss of blood during and after defecation, discontinuously (may be present for a few days, then disappear to recur another period) that do not represent a concern (everybody on constipation or diarrhea, or irritating foods, may have episodes of limited losses of blood) that however persist as long as the metal staples inside the anus are not completely eliminated (some months).
- Difficulty in retaining the gas and repeated stimuli to evacuate: It can manifest for the first 10-15 days.
- Irritation of the skin around the anus that appears red and causes itching and burning. It manifests itself in people with sensitive skin and is caused by the use of gauze, op absorbent from local ointments. It is treated with Zinc Oxide protective creams.
- Fever (up to 38 ° C) in the first days after surgery